Past Issues
Extracorporeal Shock Wave Combined with Traditional Chinese Medicine Bone-setting Manipulation for External Humeral Epicondylitis: A Randomized Clinical Trial
Changsui Yu1, Liguo Zhu2, Xiaofeng Zhang3, Zhongbao Yu4, Fengyuan Zhan4, Xin Yu5, Shuren Wang6, Kejian Lu2, Junjie Li2, Xinyue Zhang2, Daoxiong Gong7, Zifeng Xu8,*
1Wangjing Hospital of CACMS, China Academy of Chinese Medical Sciences, Beijing 100102, China
2Power Teaching Hospital of Capital Medical University, Beijing 100073, China
3Heilongjiang Provincial Administration of Traditional Chinese Medicine, Harbin 150030, China
4Liaoning Yuzhongbao Chinese Medicine Clinic, Kuandian 118200, China
5Affiliated to Guangzhou University of Traditional Chinese Medicine, Guangzhou 510405, China
6The First Affiliated Hospital of Heilongjiang University of Chinese Medicine, Harbin 150001, China
7Beijing University of Technology, Beijing 100124, China
8Health News, Beijing 100027, China
*Corresponding author: Zifeng Xu, Health News, Beijing 100027, China, E-mail: [email protected]
Received Date: July 12, 2024
Publication Date: August 06, 2024
Citation: Yu C, et al. (2024). Extracorporeal Shock Wave Combined with Traditional Chinese Medicine Bone-setting Manipulation for External Humeral Epicondylitis: A Randomized Clinical Trial. Traditional Medicine. 5(2):23.
Copyright: Yu C, et al. © (2024).
ABSTRACT
Objective: The purpose of this study was to evaluate the clinical efficacy of extracorporeal shock wave combined with traditional chinese medicine bone-setting manipulation for external humeral epicondylitis. Methods: Ninety-two patients with external humeral epicondylitis were randomly divided into an observation group and a control group. Patients in the control group were treated with extracorporeal shock waves while those in observation group with traditional chinese medicine bone-setting manipulation on the basis of the control group. Patients in both groups were evaluated by Visual Analogue Scale (VAS), Mayo Elbow Performance Score (MEPS), Disabilities of the Arm, Shoulder and Hand questionnaire (DASH) before and after treatment. The inflammatory factors such as IL-6, IL-10, TNF-ɑ and clinical outcomes were contrasted before and after treatment. Results: There were statistically significant differences in VAS score, MEPS score, and DASH score between the two groups before and after treatment (P<0.05). The observation group exhibited a more pronounced improvement in each score compared to the control group. Post-treatment, the inflammatory factors of both groups were significantly lower than pre-treatment levels (P<0.05), with the observation group showing a more noticeable decrease. The overall effectiveness of the observation group was higher than that of the control group, and the difference was statistically significant (P<0.05). Conclusion: The combination of extracorporeal shock wave therapy and traditional Chinese medicine bone-setting manipulation can effectively alleviate pain symptoms and improve dysfunction caused by external humeral epicondylitis, while also reducing inflammatory factor expression. This combined treatment may prove more effective than extracorporeal shock wave therapy alone.
Clinical Trial: Registration: ChiCTR2200066075.
Keywords: Extracorporeal Shock Wave, Traditional Chinese Medicine Bone-Setting Manipulation, External Humeral Epicondylitis, A Randomized Clinical Trial.
INTRODUCTION
External humeral epicondylitis, commonly referred to as tennis elbow, is an aseptic inflammatory condition resulting from dorsiflexion of the wrist or excessive rotational movements of the forearm [1-3]. Its principal symptoms include pain in the elbow, weakness, and limited range of motion [4,5]. In everyday life, it tends to occur more often in the 30–60 age bracket. There are numerous clinical modalities for managing this condition, including non-steroidal anti-inflammatory drugs (NSAIDs), massage, and physiotherapy (including exercise, transcutaneous electric nerve stimulation, etc.). However, the symptoms often reappear after treatment [6]. Extracorporeal shock wave therapy (ESWT), a non-invasive treatment, has demonstrated effectiveness in recent years for musculoskeletal soft tissue disorders such as humeral epicondylitis. In 2002, the Food and Drug Administration (FDA) approved the use of shock waves for treating lateral epicondylitis of the humerus. ESWT can expedite the absorption of inflammation in the surrounding tissues at the lesion site. It can also enhance the production of β-endorphin and suppress the release of associated pain factors like prostaglandin E2 (PGE2) and 5-hydroxytryptamine (5-HT), thereby achieving the goal of pain relief [7,8]. In this study, traditional chinese medicine bone-setting manipulation is one of the main methods for the treatment of meridian diseases. The main hypothesis of our study is the complementary synergistic effect of bodily functions mediated by the integration of two different alternative therapies. If this hypothesis holds true, the concurrent utilization of traditional chinese medicine bone-setting manipulation and extracorporeal shock wave therapy alongside standard care could enhance patient outcomes for individuals with lateral epicondylitis [9]. To investigate the clinical efficacy of combining traditional Chinese medicine and Western medicine in treating this condition, this retrospective study examined 120 patients with lateral humeral epicondylitis to assess the treatment effectiveness of extracorporeal shock wave therapy combined with traditional chinese medicine bone-setting manipulation.
MATERIALS AND METHODS
Clinical Information
Sample Size Estimation
The sample size underwent a two-sided hypothesis test, with the test criterion set at a=0.05 (two-sided), and test validity at β=0.10. Based on the initial observations of a small sample, the treatment group showed an efficacy rate of 95% while the control group showed a rate of 66%. As a result, it was determined that a minimum of 34 cases would be required for each group. With the incorporation of a 20% reduction in case occurrences, there were 61 instances in each cohort, yielding a combined sample size of 122. A total of 122 participants were enrolled and allocated into intervention and control groups in a 1:1 ratio to demonstrate statistical disparities and assess generalizability.
Sample Sources
One hundred twenty patients with lateral epicondylitis, who were treated at the Wangjing Hospital of CACMS and Power Teaching Hospital of Capital Medical University from January 2022 to December 2022, were included in the study. Ultimately, one case in the control group dropped out due to receiving other treatments that might affect the efficacy during the study.This research was officially designated as a clinical trial in China (ChiCTR2200066075) and given the green light by the Ethics Committee of Heilongjiang Provincial Administration of Traditional ChineseMedicine(2022KYLL089). The data pertaining to the age, duration of the disease, and the site of the disease in the participants was documented in Table 1.
Research Design
A random number table is utilized to produce a randomized assignment sequence. The research team managed the random numbers and grouping information for clinical participants. Before the commencement of clinical intervention, random numerical values and grouping data were inserted into sequentially numbered envelopes. It is challenging to blind the patients, but the trial effectively blinded the care providers and scale evaluators.
Table 1. Comparison of General Information Between the Two Groups of Patients
|
Group |
N |
Site of Disease |
Age (Years X̄ ±S ) |
Duration of Illness (Months X̄ ±S ) |
|
|
Left |
Right |
||||
|
Observation group |
60 |
25 |
35 |
40.32±6.68 |
3.18±1.19 |
|
Control group |
60 |
23 |
37 |
40.70±5.59 |
3.30±1.19 |
|
t /χ2 values |
|
0.139 |
0.341 |
0.539 |
|
|
P -value |
|
0.709 |
0.734 |
0.591 |
|
Diagnostic Criteria
All patients fulfilled the diagnostic criteria specified by the Practical Orthopaedics, published by the People’s Military Medical Publishing House [10]. (i) The forearm extensor muscles have a history of chronic injury; (ii) The individual reports experiencing lateral elbow joint pressure pain, with possible radiation of pain to the forearm. (iii) The forearm extensor group displayed positive tension during the test, along with a positive Mills sign. (iv) Imaging of the elbow joint to rule out any bony abnormalities.
Inclusion and Exclusion Criteria
Inclusion criteria: ① meeting the above diagnostic criteria; ②The illness lasts for less than 6 months and has recurring episodes. ③ 20–50 years; ④participation in this study is voluntary, and signing of an informed consent form is required.
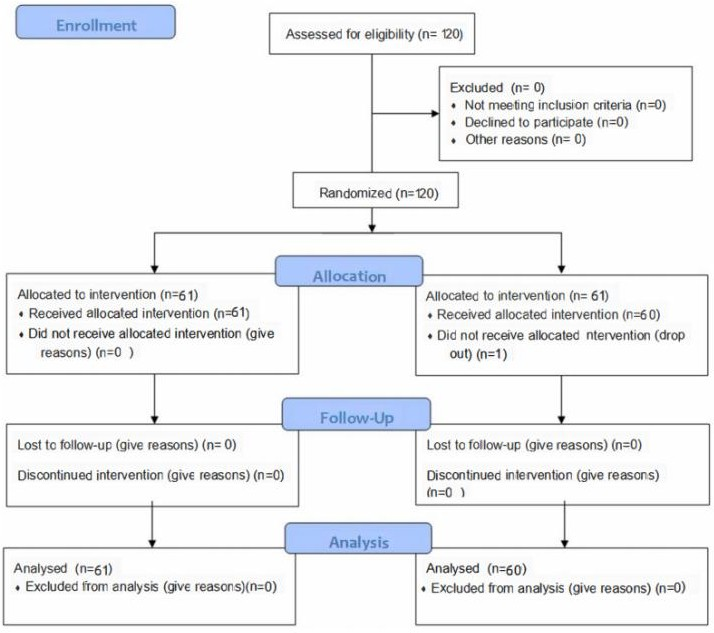
Exclusion criteria: ① combined with rheumatism, rheumatoid or joint fracture or stiffness; ② combined with serious liver or kidney disease or psychiatric disease; ③ patients who are not treated as prescribed or lost in the middle of the study. The screening process for enrolled patients is detailed in Figure 1.
Treatment Measures
The experimental treatment employed the following extracorporeal shock wave device models (Swiss Dolor Clast). The treatment utilized the following parameters: a 15mm standard probe with a parameter setting pressure of 2–3 bar, a frequency of 4–6 Hz, and a pulse of 1000–2000 times per cycle. The applicator is used to lessen tissue resistance on the patient's skin. The tender point adjacent to the lateral epicondyle of the humerus was targeted, and the intervention was administered weekly for 4 weeks, totaling 4 sessions. (Figure 2a and b).
The observation group was treated with traditional chinese medicine bone-setting manipulation on the basis of the treatment of the control group. Method operation, divided into 4 stages: (1) Rotate. The patient was sitting. The entire process of the assistant was stood on the side of the elbow, holding the remote end of the upper arm with both hands, and continuously traction with the surgeon. The surgeon is in front of the patient, holding the wrist in one hand, holding the elbow joint with one hand, and pressing the thumb on the mortar on the outside of the humerus. The surgeon shakes the front arm of the affected side 6 times, and at the same time, the thumb is gently pressed and twisted the elbow on the outside of the humerus, so that the elbow joint activity is fully relaxed. (2) Flexion phase. The arter's hand -held wrist joints slowly flexed the elbow joint of the patient three times, and at the same time, the surgeon's thumb was pulled to the remote end of the limb on the outside of the elbow. (3) The front phase. The surgeon shake the front arm of the affected side 6 times in front of the body, and at the same time, the surgeon's thumb is twisted on the outside and the elbow muscles. (4) Pulling up. The surgeon holds the side wrist joint to pull the patient's elbow joint once and stretch once. During the straight process, the thumb is poked at the outside of the outside. The technique is over. Once every other day, three times a week for a total of 4 weeks. (Figure 2c).
Efficacy Observation
Primary Outcome Indicator
Visual Analog Scale (VAS): [12] Pain intensity was measured using a visual analog scale (VAS) at a 10 cm level following wrist dorsal extension, represented by a score ranging from 0 to 10. A score of 0 indicated no pain, while a score of 10 represented the most severe and unbearable pain.
Secondary Outcome Indicators
- MAYO elbow performance score (MEPS): [13] The evaluation includes an assessment of elbow pain,range of motion, and stability, yielding a total score of 100 points. Ratings are as follows: excellent(90 or above), good (75–89 points), fair (60–74 points), poor (less than 60 points), with lowerscoresindicatingmore severedysfunction.
- The Disabilities of the Arm, Shoulder and Hand Scores (DASH) [14] range from 0 (indicating no disability) to 100 (indicating the most severe disability). The higher the score, the lower the functional ability.
- Inflammatory factor level: Fasting peripheral venous blood was collected from patients prior toand immediately after the intervention, and serum inflammatory markers including interleukin 6(IL-6),interleukin10(IL-10),andtumornecrosis factoralpha(TNF-a)wereassessed.
Effectiveness Evaluation Indicator
Efficacy assessment criteria: Refer to the "Diagnostic Efficacy Criteria for Chinese Medical Evidence" [15] for evaluation. The efficacy index is determined by dividing the pre-treatment symptom score by the post-treatment symptom score and then multiplying by 100%.
Clinical control: The symptoms and signs of the patient have either completely disappeared or significantly reduced, and the efficacy index is ≥ 90%.
Significantly effective: The patient's symptoms and signs showed significant improvement, with an efficacy index ranging from 70% to less than 90%.
Effective: The patient's symptoms and signs have shown improvement, with an efficacy index ranging from 30% to less than 70%.
Ineffective: There has been no notable improvement in symptoms and signs, with an efficacy index of less than 30%.
Total effective rate = (number of clinical control cases + number of apparently effective cases + number of effective cases)/total number of cases x100%.
Statistical Analysis
SPSS 22.0 was utilized for the analysis in the study. All outcome measures were evaluated at baseline prior to the commencement of treatment, at the conclusion of treatment, and during the 1- and 3-month follow-up assessments. The data was evaluated for normal distribution using the Shapiro-Wilk test. Descriptive data were presented as the mean ± standard deviation (SD), with a confidence interval set at 95%. Categorical variables were analyzed using chi-square tests, while unpaired t-tests were employed for continuous variables at baseline. Repeated measure analysis of variance was employed to examine the disparities in biomarker levels and functional outcomes between the two groups at various follow-up time points, while the unpaired t-test was employed to assess the distinctions between the two groups. Missing values are addressed through the utilization of a mixed linear model. P<0.05 was considered statistically significant.
RESULTS
General Information
92 patients were enrolled in the study, with 34 affected on the left side and 47 on the right side The age of participants ranged from 21 to 48 years with a mean age of 41.69 ± 5.52 (years).The duration of the disease ranged from 1 to 5 months with a mean duration of (3.46 ±1.32) months. Table 1 indicated that there were no statistically significant differences (p > 0.05) in the general information of patients between the two groups.
Primary Outcome
Comparison of VAS Scores Between the Two Groups of Patients Before and After Treatment at Various Time Periods
As depicted in Table 2, there was no significant difference in VAS score between the two groups between the two groups (p > 0.05). The VAS scores significantly improved at each time point after treatment compared to those before treatment and the difference was statistically significant (p < 0.05).At each time point after treatment ,the VAS scores of the observation group significantly improved compared to those of the control group and the difference was statistically significant (p < 0.05).
Secondary Outcome
Comparison of MEPS Score and DASH Score Between the Two Groups of Patients Before and After Treatment at Various Time Periods
Table 2. Comparison of VAS Score Between the Two Groups of Patients Before and After Treatment (Points)
|
Group |
N |
Before Treatment |
At the End of the Treatment |
1 Month After Treatment |
3 Months After Treatment |
|
VAS Score |
VAS Score |
VAS Score |
VAS Score |
||
|
Observation group |
60 |
5.12±2.39 |
2.35±1.41 |
1.84±1.18 |
1.74±1.15 |
|
Control group |
60 |
5.05±2.30 |
3.49±1.68 |
3.01±1.71 |
2.99±1.741 |
|
t-value |
0.155 |
4.024 |
4.351 |
4.704 |
|
|
P-value |
0.877 |
<0.001 |
<0.001 |
<0.001 |
Table 3. Comparison of MEPS Score and DASH Score Between the Two Groups of Patients Before and After Treatment (Points)
|
Group |
N |
Before Treatment |
At the End of the Treatment |
1 Month After Treatment |
3 Months After Treatment |
||||
|
MEPS |
DASH |
MEPS |
DASH |
MEPS |
DASH |
MEPS |
DASH |
||
|
Observation group |
60 |
49.10±5.25 |
72.82±5.14 |
80.33±5.35 |
18.31±5.25 |
84.08±4.97 |
14.82±4.85 |
84.90±4.74 |
14.62±4.74 |
|
Control group |
60 |
48.53±5.8 |
72.35±4.64 |
70.45±5.2 |
37.23±5.3 |
77.33±5.48 |
32.35±5.33 |
77.38±5.62 |
30.18±5.40 |
|
t-value |
0.601 |
0.522 |
10.434 |
20.144 |
7.067 |
18.856 |
7.916 |
16.784 |
|
|
P-value |
0.549 |
0.603 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
<0.001 |
|
Table 4. Comparison of Inflammatory Factor Levels Between the Two Groups Before and After Treatment
|
Group |
N |
Before Treatment |
At the End of the Treatment |
||||
|
IL-6 (ng/l) |
IL-10 (ng/l) |
TNF-ɑ (ng/l) |
IL-6 (ng/l) |
IL-10 (ng/l) |
TNF-ɑ (ng/l) |
||
|
Observation group |
60 |
17.63±2.79 |
18.52±2.81 |
54.18±4.01 |
6.93±2.40 |
8.52±2.68 |
26.92±3.44 |
|
Control group |
60 |
18.05±3.19 |
18.10±2.97 |
53.83±3.70 |
13.98±3.36 |
13.15±3.03 |
37.90±3.66 |
|
t-value |
0.763 |
0.789 |
0.497 |
13.233 |
8.867 |
16.941 |
|
|
P-value |
0.447 |
0.432 |
0.62 |
<0.001 |
<0.001 |
<0.001 |
|
Table 5. Comparison of Clinical Outcomes Between the Two Groups [n(%)]
|
Group |
N |
Clinical Control |
Visible Effect |
Effective |
Invalid |
Total Effective Rate (%) |
|
Observation group |
60 |
30(50%) |
15(25%) |
10(16.67%) |
5(8.33%) |
55(91.67%) |
|
Control group |
60 |
16(26.67%) |
15(25%) |
14(23.33%) |
15(25%) |
45(75%) |
|
χ2 |
6 |
|||||
|
P |
0.014 |
Comparison of Inflammatory Factor Levels Between the Two Groups Before and After Treatment
There were no statistically significant differences in IL-6, IL-10, TNF-α, and other inflammatory markers between the two groups prior to treatment, as indicated in Table 4 (P>0.05).After the intervention, the enhancement of inflammatory markers in both cohorts surpassed the pre-treatment levels, and the disparity was statistically significant (P<0.05).At the same time, the observed group showed better improvement in inflammatory indicators compared to the control group, and the difference was statistically significant (P < 0.05).
Effectiveness Evaluation Outcome
Comparison of Clinical Outcomes Between the Two Groups of Patients
According to the data presented in Table 5, there was a statistically significant difference (P<0.05) in the overall effective rate between the observation group (92.7%, 38/41) and the control group (75.0%, 30/40).
DISCUSSION
Extracorporeal shockwave therapy generates acoustic pulses of varying energy, leading to distinctive biophysical effects in human tissue, especially in chronic tendinopathies [16-18]. Patients treated with extracorporeal shock wave therapy exhibited diverse levels of enhancement in both pain management and joint mobility throughout this investigation. Compared to traditional Chinese medicine bone-setting manipulation, extracorporeal shock wave therapy has a more indirect stimulatory effect on acupoints or tender points, with relatively limited options for probe selection and energy delivery. Therefore, this study integrated traditional Chinese medicine bone-setting manipulation treatment, enabling direct action on the tender points.
This study thus incorporated traditional Chinese medicine bone-setting manipulation therapy, allowing for direct intervention at the sensitive points [19]. In order to achieve the effect of "without obstruction, without pain. "Therefore, this study employs the concept of "pain as acupuncture point" and the integration of extracorporeal shock wave and warm acupuncture therapy, representing a novel integrated approach to Chinese and Western medicine treatment.
During this investigation, we discovered that the combination of extracorporeal shock wave therapy with traditional Chinese medicine bone-setting manipulation and extracorporeal shock wave therapy alone were both successful in treating lateral epicondylitis over the 3-month observation period. However, the combined approach was more effective in alleviating pain and improving function compared to extracorporeal shock wave therapy alone. Furthermore, the combined approach exhibited superior results in terms of reducing inflammatory factor expression when compared to extracorporeal shock wave therapy alone. This evidence suggests that extracorporeal shockwave therapy, primarily through pressure load application, enhances extracellular matrix conversion, promotes neovascularization, and accelerates inflammation and catabolism, ultimately aiming to alleviate pain [20,21]. Traditional Chinese medicine bone-setting manipulation activates the meridians and channels, disperses cold, invigorates blood, and soothes the tendons and anxieties [22]. Lateral epicondylitis, also known as tennis elbow, is a chronic condition characterized by pain in the outer part of the elbow. This pain can radiate down the forearm and affect the mobility of the elbow joint to varying degrees [23,24].
The primary mechanism involves the use of extracorporeal shock waves to expedite the absorption of inflammatory substances in the tissues surrounding the lesion, suppress the release of pertinent inflammatory factors, and notably enhance the healing and regeneration of muscles, bones, tendons, ligaments, and other soft tissues. This leads to pain relief and improved mobility [25-27].
In clinical practice, Traditional Chinese medicine bone-setting manipulation is primarily utilized for the treatment of meridian tendon disorders, with pressure points as the origin of soft tissue pain. Combining the two can improve local blood circulation, enhance metabolic disorders, and reduce inflammation.
The study findings demonstrated that the integrated protocol notably decreased pain at the injury site and enhanced limb mobility in individuals with external humeral epicondylitis, a result further corroborated during subsequent follow-up and assessment. The author asserts that prompt pain relief is a crucial method to enhance the quality of life for patients with lateral humeral epicondylitis.
The study demonstrated that the combined treatment regimen was more effective for treating lateral epicondylitis.
In summary, the integration of traditional Chinese bone-setting manipulation and moxibustion treatment with modern rehabilitation medicine techniques enhances treatment efficacy and patient acceptance in orthopaedic care.
LIMITATIONS
In this study, no multi-center trial was conducted, and the sample size was small. Additionally, no blank control group was set. The study only compared the effects of a single external shock wave and the Traditional Chinese Medicine bone-setting manipulation combined with extracorporeal shock wave therapy.
Therefore, we believed that the interventions received by the control group would aid in overcoming the "Hawthorne effect."
CONCLUSIONS
This study demonstrates that the combination of extracorporeal shock wave therapy and Traditional Chinese Medicine bone-setting manipulation effectively alleviates pain symptoms and dysfunction in lateral epicondylitis. It also reduces the expression of inflammatory factors, with better results than using extracorporeal shock wave therapy alone. This combined approach is more readily accepted by patients and warrants further clinical promotion.
The team plans to undertake additional rigorous prospective randomized trials on this subject in future research to further validate the existing findings and offer more dependable scientific evidence.
REGISTRATION
The study was registered in the Chinese Clinical Trial Registry (registration no. ChiCTR2200066075).
DATA SHARING STATEMENT
The datasets created and/or examined during the ongoing study can be obtained from the corresponding author upon reasonable request.
ETHICS STATEMENT
This study has been approved by the Ethics Committee of Power Teaching Hospital of Capital Medical University within which this study was undertaken. And that it conforms to the provisions of the Declaration of Helsinki. The treatment scheme adopted in this clinical study is simple and safe. The data obtained remain anonymous. The collection of research data complies with national laws, regulations, and social ethics.
FUNDING
The work supported by Wangjing Hospital of CACMS and Power Teaching Hospital of Capital Medical University.
DISCLOSURE
The authors declare that they have no competing interests.
REFERENCES
- Chen JX, Liu GH, Liu BZ, et al. (2017). Efficacy of centrifugal contraction training combined with extracorporeal shock wave therapy in the treatment of tennis elbow. Chin J Phys Med Rehabil. 39(7):534-536.
- Zhao L, Kong LY, Ren YZ, et al. (2017). Advances in the study of humeral epicondylitis. J Pract Orthod. 23(10):904-907.
- Krogh TP, Fredberg U, Stengaard-Pedersen K, Christensen R, Jensen P, Ellingsen T. (2013). Treatment of lateral epicondylitis with platelet-rich plasma, glucocorticoid, or saline: a randomized, double-blind, placebo-controlled trial. Am J Sports Med. 41(3):625-635.
- Rabago D, Lee KS, Ryan M, Chourasia AO, Sesto ME, Zgierska A, et al. (2013). Hypertonic dextrose and morrhuate sodium injections (prolotherapy) for lateral epicondylosis (tennis elbow): results of a single-blind, pilot-level, randomized controlled trial. Am J Phys Med Rehabil. 92(7):587-596.
- Li X, Zhou K, Zhang E, Qi Z, Sun W, Xu L, et al. (2014). Therapeutic effect of electroacupuncture, massage, and blocking therapy on external humeral epicondylitis. J Tradit Chin Med. 34(3):261-266.
- Wang F, Liu JF, Zhang JT. (2022). Clinical observation on the treatment of humeral epicondylitis with external shock wave combined with thermal acupuncture in the external epicondyle and infraspinatus of the humerus. Chin J Phys Med Rehabil. 44(4):331-333.
- Xing CY. (2007). Extracorporeal Shock Wave Therapy for Bone and Muscle Diseases. 2nd ed. Beijing: People’s Military Medical Press. p. 1-4.
- Zhao D, Zhang F, Wang B, et al. (2019). Professional committee of shockwave medicine, Chinese society of research hospitals. guidelines for extracorporeal shock wave therapy for bone and muscle diseases in China (2019 edition). Chin J Front Med. 11(4):1-10.
- Peng Z, Zhang M, Li Y, Feng Z. (2020). Treatment of lateral epicondylitis with acupuncture and glucocorticoid: a retrospective cohort study. Medicine. 99(8):e19227.
- Xu ST, Ge BF, Xu YK. (2012). Practical Orthopaedics. 4th ed. Beijing: People’s Military Medical Publishing House. p. 1919.
- Schulz KF, Altman DG, Moher D; CONSORT Group. (2010). CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. PLoS Med. 7(3):e1000251.
- Beyazal MS, Devrimsel G. (2015). Comparison of the effectiveness of local corticosteroid injection and extracorporeal shock wave therapy in patients with lateral epicondylitis. J Phys Ther Sci. 27(12):3755-3758.
- Dong PL, Tang XB, Wang J, et al. (2018). Efficacy of local injection of platelet-rich plasma in the treatment of humeral epicondylitis. Chin J Joint Surg. 12(5):608-613.
- Fang ZY, Xiong L, Ch GA, et al. (2016). Clinical study of extracorporeal shock wave combined with muscle energy technique for the treatment of humeral epicondylitis. China Rehabilitation. 31(5):362-364.
- State Administration of Traditional Chinese Medicine. Diagnostic and Efficacy Criteria for Chinese Medicine Illnesses. Nanjing: Nanjing University Press; 1994.
- Wang B, Wang YH, Li A, et al. (2021). Research progress of extracorporeal shock wave treatment for tendinopathy. Chinese J Rehabilitation Med. 36(10):1332-1336.
- Yao G, Chen J, Duan Y, Chen X. (2020). Efficacy of Extracorporeal Shock Wave Therapy for Lateral Epicondylitis: A Systematic Review and Meta-Analysis. Biomed Res Int. 2020:2064781.
- Rinella L, Marano F, Paletto L, Fraccalvieri M, Annaratone L, Castellano I, et al. (2018). Extracorporeal shock waves trigger tenogenic differentiation of human adipose-derived stem cells. Connect Tissue Res. 59(6):561-573.
- Li XW, Shao XM, Tan KP, et al. (2012). A preliminary investigation on the treatment of Meridian tendon disease by combining warm acupuncture with five tiger tacking acupuncture. J Zhejiang Univ Tradit Chin Med. 36(7):818-819.
- Santamato A, Beatrice R, Micello MF, Fortunato F, Panza F, Bristogiannis C, et al. (2019). Power Doppler Ultrasound Findings before and after Focused Extracorporeal Shock Wave Therapy for Achilles Tendinopathy: A Pilot Study on Pain Reduction and Neovascularization Effect. Ultrasound Med Biol. 45(5):1316-1323.
- Simplicio CL, Purita J, Murrell W, Santos GS, Dos Santos RG, Lana JFSD. (2020). Extracorporeal shock wave therapy mechanisms in musculoskeletal regenerative medicine. J Clin Orthop Trauma. 11(Suppl 3):S309-S318.
- Zhou CL, Gao H, Liang Y, et al. (2020). An analysis of Fang J Q’s “Wu Hu Qin Yang” acupuncture method for treating Meridian tendon diseases. Chin J Tradit Chin Med. 35(3):1316-1318.
- Cao JJ, Du JJ. (2020). 57 cases of epicondylitis of the humerus treated with snap acupuncture. Chinese Acupunc. 40(8):885-886.
- Zhong CY, Hu XW. (2020). Efficacy of radiated shock wave combined with small needle knife Meridian-following treatment for recalcitrant external humeral epicondylitis. Zhejiang J Integrat Chin West Med. 30(10):846-848.
- Zhou DY, Tao HH, Yang YQ, et al. (2017). Anti-inflammatory and analgesic mechanism of extracorporeal shock wave on musculoskeletal pain. J Pract Orthod. 23(7):618-21+625.
- Yu B, Chen WH, Wang RW, et al. (2016). Efficacy of intraosseous patch combined with extracorporeal shock wave in the treatment of refractory external humeral epicondylitis. Chin J Phys Med Rehabil. 38(5):381-383.
- Reed JA. (2018). Braddom’s Physical Medicine and Rehabilitation Medicine. 5th edn. Beijing: Science Press. pp. 322-324.
 Abstract
Abstract  PDF
PDF